Condom Use Data Digest
Because today, February 14, is Valentine’s Day and National Condom Day, it’s a great time to examine trends in condom use in the United States, with a focus on external condoms because of available data. Condoms are the only method of birth control that can be used to prevent sexually transmitted infections (STIs), and national guidelines recommend that sexually active individuals using more effective birth control options (e.g., IUDs, implants, birth control pills, shot, patch, ring) also use condoms if they are at risk for STIs. Because sexually active adolescents are disproportionately at risk for STIs, understanding condom use among this population is especially important.
Findings from the National Youth Risk Behavior Survey (YRBS) indicate declines in the percentage of sexually active high school students using a condom the last time they had sex, from 63% in 2005 to 54% in 2019. Additionally, in 2019, only 9% used a condom with a more effective method of contraception. Similar trends have been documented among women of reproductive age. According to the National Survey of Family Growth (NSFG), in 1995, 20% of women reported using condoms as their most effective contraceptive method compared with 16% in 2006-2010 and 8% in 2017-2019. Estimates from 2017-2019 indicate that condoms are the fourth most popular method among women using contraception behind female sterilization, male sterilization, and oral contraceptive pills. A recent study examining young men who have sex with women found declines in condom use the last time they had sex from 2002 to 2011-2017 among those with STI risk factors.
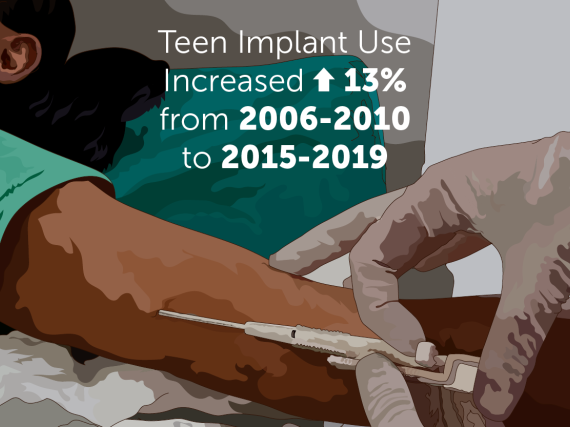
It is not entirely clearly what explain declines in condom use, although there are a number of potential reasons. One possibility is that individuals are choosing to use other methods of birth control. YRBS findings indicate an increase in use of more effective methods among sexually active students, from 25% in 2013 to 31% in 2019. Similarly, an analysis of 2007-2014 NSFG data from women aged 15-19 years found that declines in adolescent births and pregnancy rates were driven by changes in contraceptive use, including increasing use of withdrawal in combination with another method and IUDs and implants or long-acting reversible contraception (LARC). Research indicates that LARC users are less likely to use condoms compared to users of moderately effective contraceptive methods (i.e., birth control pills, shot, patch, ring).
Another possibility is the evolving context of the US HIV epidemic. Increases in condom use seen during the late 1990s and early 2000s were likely influenced by widespread HIV prevention efforts. Now there are more prevention tools available (e.g., pre-exposure prophylaxis) and a particular focus on ensuring men who have sex with men are aware of and have access to these strategies. This explanation also ties into the state of sex education in this country, which may be a contributing factor. Inclusive sex education includes information about consent, anatomy, sexual development, gender identity and expression, sexual orientation and identity, sexual and reproductive health, and much more. However, a recent analysis of NSFG data found that only about half of young people received sex education that meets minimum national standards. Additionally, a recently published study examining trends in teaching sexual and reproductive health topics in secondary schools in 38 states found few improvements between 2008 and 2018.
Despite these concerning trends, it’s worth celebrating that condoms are a widely available, affordable birth control option that can be used to prevent unintended pregnancy and STIs. Check out this resource from Power to Decide on the many benefits of condoms that we can share as part of efforts to ensure sexual and reproductive well-being for all.