The Great Hormone Debate
In recent years debate has increased about hormonal vs non-hormonal birth control options. Is there a best method? Or a correct answer? Of course not; no one birth control method will always work for all people. Birth control, like many other aspects of life, is a journey. In fact, on average, women in the United States use five different birth control methods throughout the course of their lives.
What Are Hormones?
There are a number of different types of hormones, but essentially, they are all chemicals made in one part of a living thing that travel to another part, affecting it. Though there are many sex hormones, the most common are estrogen, progesterone, and testosterone. For people with ovaries, during puberty the body begins to make estrogen and progesterone in large amounts. The graph below illustrates how hormone levels fluctuate in the average female between age 15-40 who isn’t using hormonal birth control.
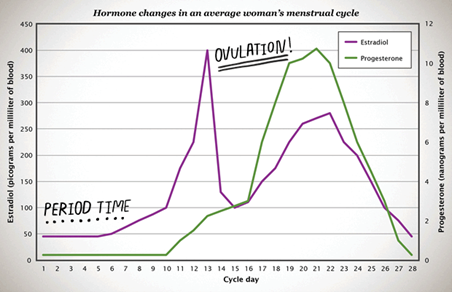
While estrogen and progesterone aren’t the only hormones involved in a menstrual cycle, they are the two that cause either a period or a pregnancy. Both increase approximately ten times over the course of a few days around the time an egg is released from the ovary. The amount of estrogen and progesterone an individual makes and the timing in which amounts increase changes from cycle to cycle depending on lots of factors such as age, health, and stress level.
How Does Hormonal Birth Control Work?
The hormones in some methods of birth control are similar to the ones bodies make on their own—close enough that the body recognizes them as estrogen and progesterone. There are multiple kinds of hormonal birth control, each with unique ingredients that are released differently. For example, how do the hormonal IUD and the combination pill work to prevent pregnancy?
Hormonal IUDs
Hormonal IUDs release a small amount of levonorgestrel—a progestin hormone—nearly all of which stays in the uterus. Levonorgestrel is one of the longest-studied types of progestin, and all the scientific evidence to date shows it’s super safe. The amount of levonorgestrel released by these IUDs stays very steady day-to-day but declines slowly after the first year. The main way hormonal IUDs work to prevent pregnancy is by keeping cervical mucus thick so sperm can’t get through the cervix to meet with an egg. These progestin hormones vary in potency, but even the highest levels of progestin in these methods of birth control are lower than the average natural monthly spike of progesterone produced by the body. The way a person’s IUD impacts their body varies slightly based on the type of IUD they have; most folks using Skyla have their usual changes in estrogen and progesterone each cycle, and most release an egg each month. People with a Mirena IUD typically have their usual hormonal cycles after a year and still release an egg.
The Pill
While there are numerous different brands of the combined pill, all must be taken once a day at the same time and they all contain both estrogen and a progestin. The average amount of hormones from the pill in a person’s blood ranges, as the graph below shows. Levels peak about two hours after the pill is ingested and before decreasing. Within 36 hours the body has cleared all of the hormones, which is why the pill must be taken every day in order to prevent pregnancy.
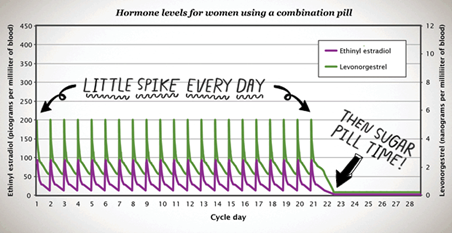
In general, when on the pill, the body makes less of its own progesterone and estrogen. Pill users don’t make their own spike of progesterone, nor do they release an egg. Because different brands of the pill use different types and amounts of hormones, if one doesn’t work—for whatever reason—another brand with different ingredients or hormone levels may be a better option.
Hormonal Contraception vs Non-Hormonal Contraception
Everyone’s body is unique and a method that doesn’t work for one person might be perfect for another. That means it’s difficult to make a blanket statement about how hormones impact people. Plus, studies on the relationship between sex hormones in people with ovaries and potential side effects often have mixed results. So, what are some of the reasons that people prefer hormonal or non-hormonal contraception?
Hormonal methods of birth control can help:
- Reduce or eliminate heavy or painful periods.
- With acne.
- With ovarian cysts.
- Reduce the risk of ovarian cancer.
- Control gender dysphoria.
Side effects experienced by some folks when using hormonal contraception include:
- Spotting.
- Headaches.
- Nausea.
- Sore breasts.
- Changes to sex drive.
While research hasn’t found any clear answers, some people also report gaining or losing weight while on hormonal contraception and others describe entering or exiting a depression. The only exception to this grey area is with the shot where research has found a connection between usage and weight gain.
Many side effects fade as a person’s body adjusts to a new method, so it can be worth holding out for around six months to judge if things improve or even out.
Hormonal contraception is safe to use for any length of time, but it’s not for everyone. Those who prefer a non-hormonal birth control option have several to choose from; the copper IUD is the most effective, but there are also condoms, the diaphragm, and fertility awareness methods.
Folks can choose from 18 categories of FDA-approved birth control methods, but not all methods are right for everyone all the time. All people deserve unfettered access to the method of birth control that they and their trusted medical provider determines is right for them at that time. And with so many different birth control methods out there, there’s something for everyone. The only way to find out how a method will work with your body and lifestyle is to talk to a health care provider and try different options until you find the perfect match.