What to Do If You Are Having Trouble Getting No-Copay Birth Control
On January 10, the Biden-Harris administration issued guidance to ensure insurance plans cover the specific method of birth control people and their providers need, without co-pays or deductibles. The additional Guidance on the Birth Control Benefit (scroll to page 12) outlines ways in which insurance plans have potentially violated the contraceptive coverage requirements of the ACA and was released in direct response to stakeholder feedback. Potential violations outlined include insurance plans denying coverage even after a health care provider communicates the necessity of a particular brand name or type of birth control, requiring people to “fail first” meaning use non-preferred methods of birth control or other health services prior to approving a preferred contraceptive method, and not providing an “easily accessible, transparent...sufficiently expedient...[and] not unduly burdensome on the individual or a provider” when a specific method of birth control not otherwise covered is needed.
Additionally, the guidance also directs consumers to two hotlines to report plans that are not covering their birth control as required. Those who are covered by health plans through a non-federal, public-sector employer-sponsored plan (aka if a person works for a state or local government) may contact the Health Insurance Assistance Team of the US Center for Consumer Information and Insurance Oversight at 1-888-393-2789 or phig@cms.hhs.gov.
People that are covered by private insurance through their employer and who have concerns about their plan’s compliance may contact the Department of Labor at askebsa.dol.gov or by calling toll free at 1-866-444-3272. The process to report a complaint may feel overwhelming at first, but it’s easier than it looks. However, it could be helpful for everyone—but especially people who may mentor or advise those who find themselves in a situation where they need to report their insurance plan—to take some time to understand the process.
We encourage everyone to share this information widely, especially in health care settings such as clinics, waiting rooms, and pharmacies. The more that these hotlines hear from people struggling to get their no-copay birth control, the better the understanding the government will have of with the scope of the issues to be addressed.
Broadly, to make a complaint about your private employer plan:
1. Go to askebsa.dol.gov. Click “Make a Complaint” under the “Tell Us About It Online” section. For those who would prefer to make their complaint in Spanish there is a second option; although it translates to “ask a question,” by clicking “Hace una Pregunta,” users will be redirected to a Spanish-language version of the form. While “Hace una Pregunta” translates to “ask a question” in English, choosing this option will redirect people to the Spanish language version of the English complaint form.

The next page, “Request Assistance from a Benefits Advisory” is composed of four sections.
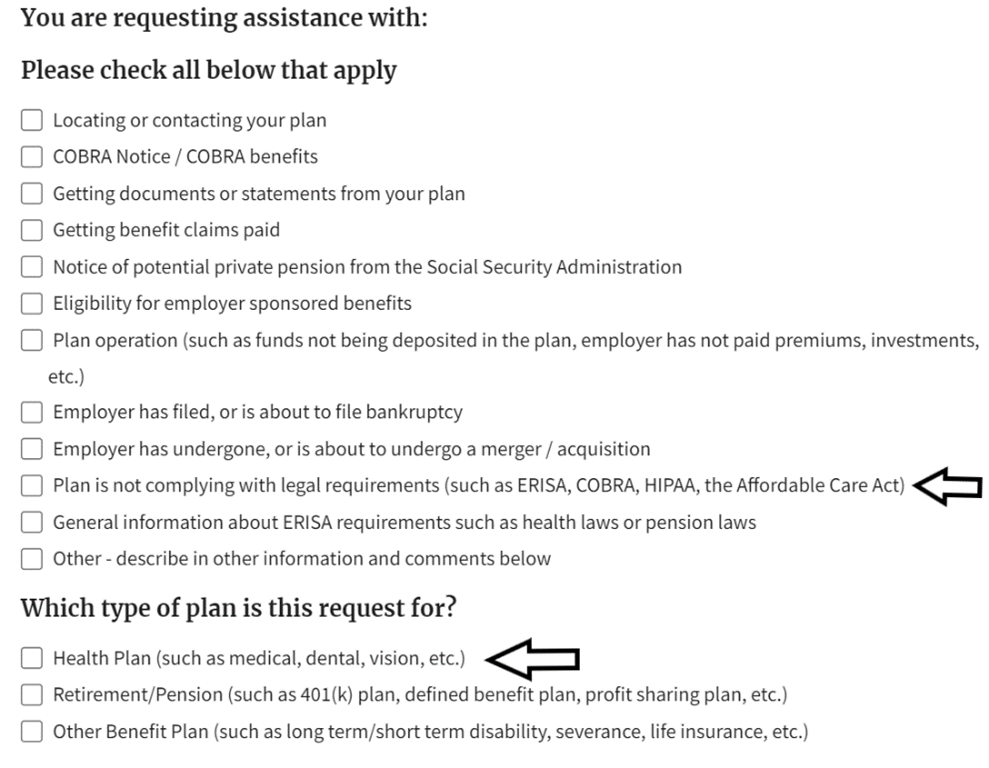
2. In section one, “Plan is not complying with legal requirements” and “Health plan” will need to be checked.
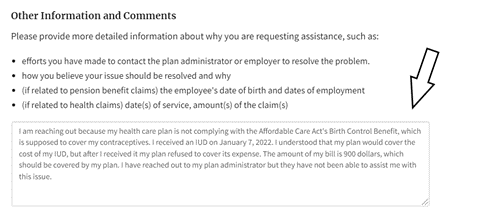
In the box beneath these questions is a space to state the circumstances under which the health plan is out of compliance. For example,
At the bottom of the page in this section you will find the answers to the FAQs “How will my information be used?” and “What happens after I submit a request for assistance?”
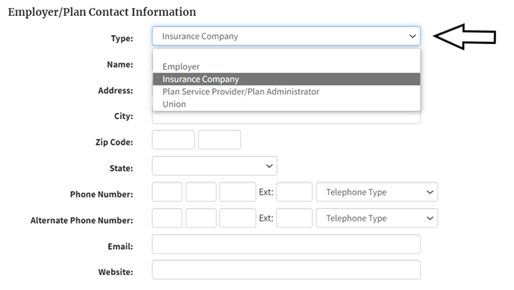
3. In the second section you can add in contact information for your insurance plan or employer. We recommend choosing “Insurance Company” in the drop down under “Type”, and then the name of your insurer for example United Health, Blue Cross Blue Shield, Cigna, Kaiser Permanente in the “Name” field below. If your prescription is being denied by what is called a pharmacy benefit manager (such as Express Scripts, Optum, and CVS Caremark) then choose “Plan Service Provider/Plan Administrator from the drop down). This information is not required but will help an advisor better assist you.
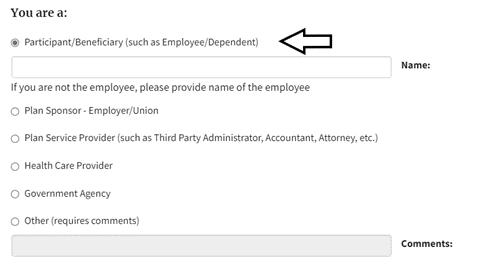
4. Section three requests personal contact information. While only first and last name, state and zip code, and phone are required, providing more information will help the Benefits Advisor provide an answer more quickly. After you put in your information you will check “Participant/Beneficiary” at the bottom of the page.
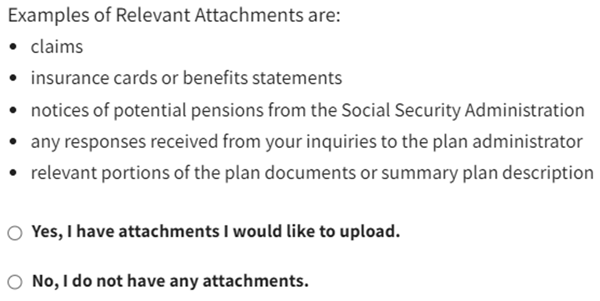
5. In the final section additional information, including attachments, about the complaint can be added. If you don’t have any additional information or documents to attach, click “No, I do not have any attachments.”
At the bottom of the page, you can click on the “Privacy Information” and “Paperwork Reduction Act Information” if you want further information on the protection of your private information submitted on the form.
6. Once the form is submitted a Benefits Advisor will contact you.
Anyone can still contact coverher.org for help getting health care coverage that includes no-cost contraception, but making sure you also report your plan for not complying with the ACA is an important step.
Sitara Sayyed is the Public Policy Intern at Power to Decide where she assists the Public Policy team with federal policy issues. She attends University of Maryland where she studies Public Policy.


